If you’re suddenly burning up from the inside out, breaking into a sweat, or tossing off the covers at 3am – welcome to one of the most recognisable signs of perimenopause, menopause and sometimes post-menopause: hot flushes. These sudden surges of heat can be unsettling, exhausting, and downright disruptive. But they’re also extremely common.
Here’s why they happen, what triggers them, and how to cool down naturally.
What Are Hot Flushes?
Hot flushes (also called hot flashes) are brief but intense feelings of heat, usually in the face, neck, and chest. Although some women describe them as a slow rising heat that starts low. And they can also be accompanied by:
- Red or flushed skin
- Rapid heartbeat
- Excessive sweating
- Anxiety or panic sensations
- Follow-up chills
They’re especially common during perimenopause – the hormonal transition phase leading up to menopause – and can occur during the day or night (when they’re called night sweats). However, for some women, they can continue for years.
Tip: experts say some instances of hot flushes in post-menopause could relate to hypertension, so it’s important to get a health check-up.
Fact: Around 75%–80% of women experience hot flushes during the menopause transition. [1]
What Causes Hot Flushes in Perimenopause?
The main culprit? Fluctuating estrogen levels.
Your brain has an internal thermostat controlled by a region called the hypothalamus. Estrogen plays a role in keeping this thermostat regulated. But when estrogen starts to fluctuate – as it does during perimenopause – the hypothalamus becomes more sensitive to tiny changes in body temperature.
Even small shifts can trigger a full-body reaction: blood vessels dilate, sweat glands activate, and suddenly you’re radiating heat like a furnace.
Fact: The truth is, experts don’t fully understand hot flushes, but researchers have found that hot flushes correlate with reduced estrogen and erratic hormone signalling in the brain’s thermoregulatory centre. [2]
It’s not just about estrogen.
- Progesterone levels are the first to decline in perimenopause, impacting sleep and increasing anxiety – both of which can worsen the experience of hot flushes.
- Cortisol, the stress hormone, tends to rise during midlife due to lifestyle and emotional demands as well as hormonal shifts. Elevated cortisol has been shown to intensify menopausal symptoms. [3]
- Thyroid issues, both overactive (hyper) and underactive (hypo) thyroid are common over 40 and can also be behind hot flushes and sweats. [4]
Tip: It’s a smart idea to have your ferritin (iron storage), vitamin D, and B12 levels checked as low levels can impact hot flushes.
Common Triggers That Worsen Hot Flushes
Even though hormones are often the underlying cause, these triggers can amplify symptoms:
- Caffeine
- Alcohol
- Spicy foods
- Tight clothing or warm environments
- Stress and anxiety
- Smoking
- Sugar and ultra-processed foods
Tip: Keeping a symptom diary can help you identify your personal triggers.

Natural Ways to Ease Hot Flushes
While hot flushes may be inevitable during perimenopause, there are powerful, natural strategies to manage them:
1. Try Phytoestrogens
Found in flaxseed, soy, lentils, and chickpeas, these plant-based compounds have mild estrogen-like effects that may help balance hormone levels. If you’re overweight or obese, use moderate levels.
Study: A review of 15 trials found that soy isoflavones reduced hot flush frequency and severity. [5]
2. Balance Blood Sugar
Unstable blood sugar can exacerbate hormonal chaos. Focus on protein-rich meals, fibre, and complex carbs to keep energy – and hormones – steady.
3. Lower Stress with Mindfulness
Stress increases cortisol and worsens flushes. Try yoga, deep breathing, or mindfulness meditation.
Fact: A 2019 study found mindfulness-based stress reduction (MBSR) improved hot flush symptoms and overall quality of life in midlife women. [6]
4. Improve Sleep Hygiene
Flushes are notorious for wrecking sleep. Try:
- Keeping your bedroom cool
- Wearing moisture-wicking pyjamas
- Using fans or cooling pillows
- Limiting alcohol and caffeine before bed
5. Hydrate Generously
Flushes = fluid loss. Stay ahead of dehydration by drinking plenty of water and eating hydrating foods (like cucumber, berries, and leafy greens). But avoid two to three hours before sleep so you’re not up and down to pee.

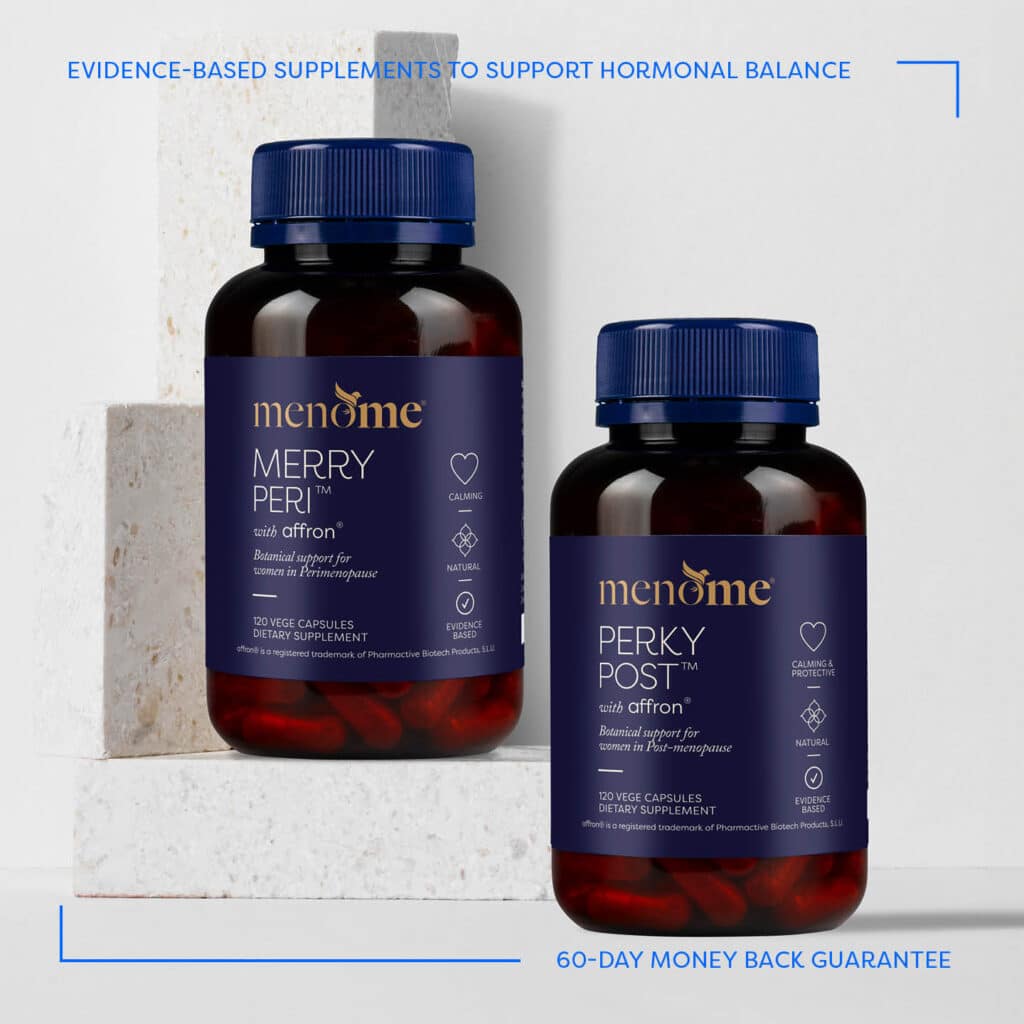
6. Add Natural Support To Your Menopause Toolkit
Merry Peri® is your go-to supplement for perimenopausal support, helping to ease hot flushes, mood swings, and stress with evidence-based botanicals like saffron, fenugreek and sage. It’s designed to work with your body, not against it, during the rollercoaster of hormonal shifts.
And then there’s Perky Post® – ideal for post-menopause, offering continued hormonal and mood support for those still experiencing flushes or emotional fluctuations after their periods have stopped.
Both formulas are part of a natural, evidence-based approach to navigating menopause with grace – and feeling more like yourself again.

In Summary: You’re Not Alone
Hot flushes can feel like an internal inferno – but they’re also a powerful signal that your body is going through a natural transition. With a little support and know-how, you can ride the wave of perimenopause and feel empowered, not exhausted.
You’ve got this – and we’re right here with you.
Disclaimer: This article is for educational purposes only and is not intended as medical advice. Always consult with your medical professional, especially if you have underlying health conditions or are taking medications.
Just so you know: this article is written by a real person who has studied the physiology of menopause and women’s healthy aging. While we may use AI as an assistant, the research, insights and heart behind every piece comes from us.
References:
Around 75–80% of women experience hot flushes during menopause.
Hot flushes stem from estrogen withdrawal and thermoregulatory instability in the hypothalamus.
Early progesterone decline, elevated cortisol rhythms, and thyroid dysfunction also intensify symptoms.
It’s wise to check ferritin, vitamin D, B₁₂, and thyroid function, as imbalances can worsen flushes.
Meta‑analyses show soy isoflavone supplements (~54 mg/day, especially ≥18.8 mg genistein) reduce hot flush frequency by ~20% and severity by ~26%.
An 8‑week MBSR program has been shown in RCTs to lower hot flash distress by ~40% and frequency by ~39%, plus improve QoL and stress.