So many of you have asked us if breast cancer is more common during menopause. And the answer is yes, because one of the highest risk factors for a breast cancer diagnosis is growing older.
“Most breast cancers occur in women over 50 years of age, so it’s important that you keep up to date with regular mammograms after turning 50 and be aware of any unusual changes happening in your breasts.” – NZBCF
Breast cancer and menopause
Although heart disease is the biggest killer of women, breast cancer is the most common type of cancer.
However, the Australasian Menopause Society suggest keeping the risk in perspective. They note that:
“The greatest risk factor for breast cancer is a family history of breast cancer in a close relative. The next major risk factor is increasing age so breast cancer under the age of 35 years is much less common than breast cancer after the age of fifty. Other risk factors such as late menopause, late first birth, HRT use and alcohol consumption are much smaller risk factors for breast cancer.”
What’s more, they also add that the benefits of diet and exercise and the associated lower risk of breast cancer are poorly understood1.
A word about estrogen receptor-positive and/or progesterone receptor-positive breast cancer

The New Zealand Breast Cancer Foundation (NZBCF) tell us normal breast cells contain receptors (proteins) that recognise these hormones and allow them access to cells, where they release signals encouraging growth and development.
In addition, all breast cancers are tested for estrogen and progesterone receptors. Approximately 70% of breast cancers rely on these hormones (particularly estrogen) to grow. These hormone-sensitive cancers are described as estrogen receptor-positive (ER+) and/or progesterone receptor-positive (PR+).
That’s certainly a powerful reason to avoid xenoestrogens and endocrine disruptors. (More on that later.)
You might like: Menopause, Hormones & Toxins
Did you know? Breast common is most common in women over the age of 50.. Share on X
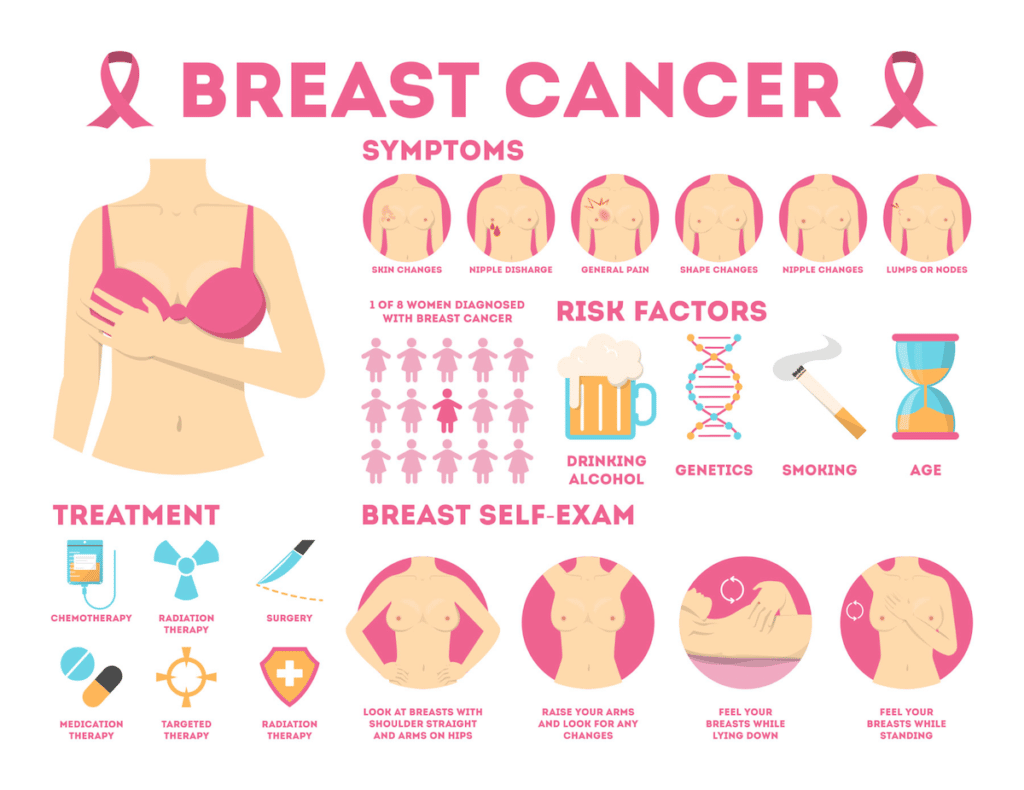
How to check for breast cancer
There’s compelling evidence behind the advice to get to know your breasts. Because there’s no doubt that the more familiar you are with them the sooner you’ll notice any changes.
TLC: Touch, Look, Check
Also, ensure you have a regular mammogram every two years. These are free in New Zealand from 45-69 and in Australia from the age of 40.
If you are younger than this your breast tissue may still be quite dense therefore the addition of an ultrasound screening is recommended.
Signs and symptoms of breast cancer
A lump in the breast is traditionally thought of as a red flag for breast cancer.
But it’s important to realise that, along with fibrocystic breasts and cysts, the majority of lumps – while disturbing – are harmless. In fact, they’re more of an indicator of overall breast health. Indeed, hormonal imbalance, estrogen dominance and high cortisol can all affect the overall health of your breasts.
So again, it’s important to keep things in perspective.
Signs and symptoms of breast cancer include:
- A lump
- Thickened breast tissue
- Changes in nipple size
- Changes in breast size or shape
- An inverted nipple
- Nipple discharge
- Dimples puckering or dents
- Orange peel-like skin
- Unusual breast pain
8 risk factors for breast cancer during menopause
1. Being a woman
Ninety-nine percent of breast cancer cases occur in females. Moreover, 75% of those present in women aged over 502. Nen can get breast cancer too but this only occurs in 1% of cases.
2. Growing older
Studies show that as we grow older our chance of developing breast cancer increases, especially after the age of 50.
3. Risk factors related to age (in the next 10 years):
- 20s – 1 in 1314
- 30s – 1 in 204
- 40s – 1 in 50
- 50s – 1 in 37
- 60s – 1 in 29
- 70s – 1 in 36

4. Family history
The potential to develop breast cancer is increased if a family member has had breast or ovarian cancer. Equally important is the family member’s age and whether they are first and second-generation relatives3. Furthermore, if you are of Ashkenazi (Eastern European) Jewish ancestry you may be more at risk2.
5. BRCA1 and BRCA2 Gene
The BRCA1 and BRCA2 genes are associated with the risk of both breast and ovarian cancer. Although, according to Australia’s National Breast Cancer Foundation BRCA1 and BRCA2 mutations are rare. About 1 in 400 to 1 in 800 people have a BRCA1 or BRCA2 gene mutation. It must be remembered that not everyone who has a faulty BRCA1 or BRCA2 gene will develop cancer. 5
6. Age of menstruation and menopause
There’s a link between the length of time a woman produces estrogen so hormonal factors come into consideration2:
- Younger age at first menstruation (under 12)
- Older age at menopause (over 55)
- Having few or no pregnancies
- A short time breastfeeding or no breastfeeding
- Later age at first childbirth i.e. women aged over 30 will have been producing estrogen continuously for longer
7. Overweight & obesity
Being overweight or obese increases risk, especially post-menopause. For one thing, carrying more weight may cause estrogen to be produced in the fat tissue. As a result, there will be more estrogen in the body. In the same way, losing weight will decrease the risk. According to Cancer Australia, 8% of breast cancers in post-menopausal Australian women are related to weight gain5.
Tip: According to the NZBCF being overweight before menopause doesn’t carry the same risk.
8. Alcohol
Did you know that drinking more than two standard drinks per day increases your risk of breast cancer? Or, the risk of breast cancer returning. And the risk increases with the number of drinks you consume5.
Moreover, the NZBCF tell us that drinking alcohol has been firmly established as a risk factor for developing breast cancer. This is because alcohol changes the way the body metabolises estrogen, causing levels to rise6.

A word about Menopause Hormone Therapy (MHT) formerly known as HRT
At this point, there is much discussion regarding breast cancer risk and hormone therapy. This includes birth control pills as well as HRT. Some experts state the breast cancer risk for modern-day HRT (MHT) is equivalent to having a glass of wine daily.
“Results from the Million Women Study, the Women’s Health Initiative Study and the Nurses Study showed that women taking combined hormone replacement therapy, using both estrogen and progestogen, had an increased breast cancer risk during use and for two to five years afterwards. The longer you use it, the higher your risk. Estrogen-only HRT (prescribed for women who no longer have a uterus) is associated with little or no change in breast cancer risk. If you’re considering using HRT, talk to your doctor about the risks versus benefits. It is recommended that HRT use should be at the lowest possible dose to control symptoms, for the shortest possible time.” The New Zealand Breast Cancer Foundation
iPrevent
This is a really good interactive online quiz by the Peter MacCallum Cancer Centre in Australia. It’s been developed to help you understand your risk of breast cancer. Click here to try it out.
Breast cancer, menopause & chemotherapy
In some instances, due to a diagnosis of breast cancer premenopause, chemotherapy treatment may put you into early menopause. Please read about early menopause here.
3 ways to keep your breasts healthy & reduce your risk of breast cancer
1. Eat your veggies
Especially the cruciferous and brassica veggie family. We often suggest upping your veggie content with lots of cruciferous vegetables pre-, peri- and post-menopause because they’re good for your health, weight and gut. But they’re also super good for your breast health. The truth is, they may be cancer preventative.
The cruciferous and brassica family include broccoli, cauliflower, kale, Brussels sprouts and kale. Cruciferous vegetables are rich in sulforaphane and diindolylmethane (DIM). This helps the body break down estrogen and supports liver detoxification by turning estrogen into a healthy estrogen metabolite (2-hydroxyestrone)3.
In fact, this study9 found that supplementing with 108 mg of DIM daily increased the 2-hydroxylation of estrogen urinary metabolites in post-menopausal women (age 50-70) who had a history of breast cancer.

2. Exercise regularly
You already know exercise is Queen for your overall health. But it also lowers the risk of breast cancer and the chances of it returning.7,8
3. Avoid xenoestrogens and endocrine disruptors
Xenoestrogens and endocrine disrupting chemicals (EDC’s) are chemicals in our environment, personal care products and cleaners that mess with hormones such as estrogen and progesterone10. To put it simply, they mimic our natural estrogen and can create an ‘overload’. Additionally, they are believed to be carcinogenic. So avoiding xenoestrogens and EDC’s is suggested to reduce risk of breast cancer.
You’ll find xenoestrogens in:
- Plastics
- Cleaning product
- Personal care products
- Skin care and makeup
Of course, waging war on the risk factors you can control like minimising alcohol and maintaining a healthy weight is smart as well.
Conclusion
Although the biggest killer of women is heart disease, the biggest female cancer risk is breast cancer.
And breast cancer and menopause are both associated with growing older. What’s more, there is a direct correlation between being a female who has a few more years around the sun and breast cancer.
Nonetheless, just because you’ve reached menopausal age it doesn’t mean you will get breast cancer. Furthermore, a diagnosis of breast cancer isn’t a life sentence as we’ve seen a significant increase in survival post-diagnosis.
And balanced against that, in many cases it’s also possible to lessen your risk of developing breast cancer.
To that end, we hope this has been helpful for you or someone you love. 💙
FREE Downloadable Resources:

Disclaimer: Our articles are for information purposes only. As such, they are not a diagnostic tool. For this reason, if you are concerned that you may have an increased risk of breast cancer please see your medical professional.
Share with a friend
Sign up to our mailing list for the latest news and stories and receive a $5 discount code to redeem on your first purchase, plus receive a 3-step eBook on ways to support your body through menopause.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Related Articles
References:
- Australasian Menopause Society menopause.org.au/health-info/self-assessment-tools/breast-cancer
- New Zealand Breast Cancer Foundation (NZBCF) breastcancerfoundation.org.nz/breast-awareness/risk-factors/risk-factors-we-can’t-change
- In The Pink: a guide to breasts, cancer and living well by Lani Lopez & Jenna Moore, Bateman, pg 31
- Tapia KA, Garvey G, Mc Entee M, Rickard M, Brennan P. Breast Cancer in Australian Indigenous Women: Incidence, Mortality, and Risk Factors. Asian Pac J Cancer Prev. 2017 Apr 1;18(4):873-884. doi: 10.22034/APJCP.2017.18.4.873. PMID: 28545182; PMCID: PMC5494235.
- National Breast Cancer Foundation Australia nbcf.org.au/about-breast-cancer/prevention-and-risk
- New Zealand Breast Cancer Foundation (NZBCF) breastcancerfoundation.org.nz/breast-awareness/risk-factors/lower-your-risk-of-breast-cancer
- CMAJ, Julia Hamer and Ellen Warner, February 21, 2017 189 (7) E268-E274; DOI: https://doi.org/10.1503/cmaj.160464
- Eliassen AH, Hankinson SE, Rosner B, Holmes MD, Willett WC. Physical activity and risk of breast cancer among postmenopausal women. Arch Intern Med. 2010 Oct 25;170(19):1758-64. doi: 10.1001/archinternmed.2010.363. PMID: 20975025; PMCID: PMC3142573.
- Dalessandri KM, Firestone GL, Fitch MD, Bradlow HL, Bjeldanes LF. Pilot study: effect of 3,3′-diindolylmethane supplements on urinary hormone metabolites in postmenopausal women with a history of early-stage breast cancer. Nutr Cancer. 2004;50(2):161-7. doi: 10.1207/s15327914nc5002_5. PMID: 15623462.
- Environmental Oestrogens and Breast Cancer: Evidence for Combined Involvement of Dietary, Household and Cosmetic Xenoestrogens, Philippa D. Darbre, Amelia K. Charles, Anticancer Research Mar 2010, 30 (3) 815-827;









