Fewer leaks? Eeep! Seriously, what are you talking about?
Actually, I’m talking about urinary incontinence and perimenopause and post-menopause. The percentage of women who experience menopause related bladder leakage is large, but nobody wants to talk about it.
Indeed, it’s as taboo as menopause used to be.
A 2011 study by the Medical University of Vienna in Austria said the issue is ‘considered significantly more embarrassing than depression or cancer’.
But we need to bring it out into the open because it happens to a lot of us. In fact, the World Health Organisation recently listed incontinence as a major health issue.
Here are a few numbers:
- Three to six million people in the UK suffer from incontinence
- 80% of Australians who live with incontinence are women
- 175,000 adult Kiwi women are bothered by a leaky bladder
- Globally, over half of the female population will experience leakage at some time in their lives
- A three-month Australian study found 50 percent of women aged 45-59 experienced mild, moderate or severe urinary incontinence.
Of those people, only about 30% seek treatment.
Those are some pretty big numbers. And while the problem isn’t life-threatening, it affects quality of life, self-esteem, sexual activity and depression. Combine that with other perimenopause and post-menopause signs, and it’s not much fun at all.
The World Health Organisation recently listed incontinence as a major health issue. Share on X
How Does The Bladder Work?
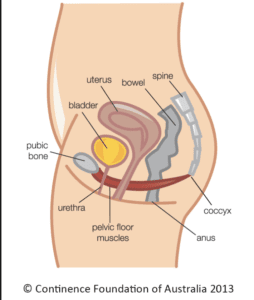
The diagram above from Continence.org.au shows us the bladder is a storage organ that sits in our pelvis. They explain that urine is made by the kidneys and stored here until we are ready to empty it. When we go to the toilet the outlet muscles (urethral sphincter and pelvic floor) relax. Then the bladder itself contracts (squeezes) emptying it of urine. Our brain controls the process by sending messages to tell the bladder when to hold and when to empty.
Common Signs Of Bladder Issues
Passing urine frequently and rushing to the toilet (urgency) to pass urine are the most common signs.
Others include:
- leakage of urine with coughs, sneezes, or exercise
- urine leaks on the way to the toilet
- getting up twice or more overnight to pass urine
- frequent urinary tract infections
- being unable to control wind
- constipation
What Happens During Perimenopause?
With age, perimenopause and post-menopause, the pelvic floor muscles begin to weaken. And as the pelvic floor is crucial to bladder control a weakness may cause more regular urges to go to the loo. Furthermore, we may have less of an ability to ‘hold on’.
Over time, the bladder also becomes less elastic. Therefore it doesn’t ‘stretch’ easily to accommodate the urine as it fills and may become irritated bringing on an urge to urinate.
Gaining weight can also create issues. A significant amount of weight gain can put strain on the pelvic floor muscles. This, in turn, exacerbates their weakened ability to support your bladder.
In fact, it can be damn uncomfortable.
With age and perimenopause, the pelvic floor muscles begin to weaken. Share on X
What Can You Do?
1. Keep your weight in a healthy range.
Carrying extra kilos adds pressure to your bladder — it’s as simple as that. Lightening the load can make a noticeable difference.
2. Watch what (and when) you drink.
Some beverages, like coffee, fizzy drinks, and alcohol, act as diuretics — meaning they fill your bladder faster and irritate it too. So, they’re best avoided if you’re struggling. Water is still your best friend; it hydrates without the side effects. Try setting a cut-off time in the evening to reduce those middle-of-the-night bathroom visits.
3. Strengthen your pelvic floor.
Pelvic floor exercises (Kegels) help tone the muscles that support your bladder — and come with plenty of other benefits! You can get the feel for them by pausing your urine mid-flow. Once you’ve mastered that sensation, practise your Kegels anytime — while sitting at your desk, driving, or brushing your teeth. Start with 10 squeezes two or three times a day and build from there.
Tip: Don’t make a habit of doing them while actually urinating — that can confuse your bladder’s natural signals.
4. Support your bladder from the inside.
Nutrients such as zinc, vitamins C and D, magnesium, and D-mannose can help. D-mannose, in particular, may reduce the risk of urinary tract infections (UTIs).
5. Use smart supports when you need them.
A pelvic floor trainer like Elvie can be a game-changer for some (read my story below). And if leaks do happen, keep your confidence with discreet pads or specially designed underwear.
My Life With Elvie

I had no idea of all of these possible changes. So when I began having untimely urges to go to the loo (when it was incredibly inconvenient), I didn’t know why. I tended to put it down to infection, but it got worse.
Kegel exercises were put on my daily to-do list, but I frequently forgot. Then I discovered Elvie.
According to the Journal of Obstetrics and Gynaecology, you need to do one hundred Kegels a day (it’s the movement you use to stop your urine midstream). Share on X
A beautifully designed, state-of-the-art pelvic floor trainer with app. It’s part of a new wave of feminine-tech offerings coming on the market designed by women for women. 😀
I can honestly say Elvie changed my life. I used it religiously at first, and as my signs improved, I used it less often to keep toned.
It definitely helped. I also avoided common bladder irritants like coffee and alcohol, and over time, things subsided and are now manageable, so I can tell you, it does get better.
Need help? Send me an e here.
With thanks to continence.org.au and continence.org.nz